by Beth Wangigi
Grace (not her real name), 47, has lived with the challenges of an untreated injury for over two decades. When she was delivering her third child, she faced a difficult delivery, laboring for hours with the assistance of a traditional birth attendant. The experience left her with a fourth-degree perineal tear, leading to stool incontinence and chronic back pain. Even daily tasks became difficult; walking or any strenuous activity would bring discomfort and shame.
See this report in it’s original, dynamic form – https://storymaps.arcgis.com/stories/01a1b7babdb24e0c9f194cd420770c84
As a peasant farmer with limited income, the idea of surgery seemed out of reach. For 22 years, Grace managed as best as she could, but her condition isolated her and kept her from fully participating in daily life. Finally, during a birth injury repair camp by AMH at Ibanda Hospital, Grace received the surgery she needed. The repair was successful, and she was discharged, grateful and relieved, with a new sense of hope and restored dignity.
Grace’s story is a reality for a lot of women. Many women in Africa endure birth-related injuries due to a combination of factors, including limited access to healthcare facilities, lack of trained personnel, and cultural practices that delay safe medical interventions.
In Sub-Saharan Africa, maternal healthcare is particularly under-resourced, leading to high rates of these preventable conditions. These often go untreated due to stigma, insufficient healthcare access, and low awareness.
It is estimated that 0.5 – 2 million women live with untreated obstetric fistula in Asia and Sub-Saharan Africa. Women who experience obstetric fistula suffer constant incontinence, shame, social segregation, and health problems. – WHO
In the year 2003, it was estimated that approximately 100,000 women live with this condition, primarily among those in poverty, with 1,900 new cases annually – Uganda Demographic Health Survey 2022
It’s estimated that only around 3% of women suffering from obstetric fistula seek medical treatment. This low figure is due to multiple barriers, including lack of awareness, financial constraints, social stigma, and limited access to specialized fistula repair services, particularly in rural regions.- Uganda National Obstetric Fistula Strategy
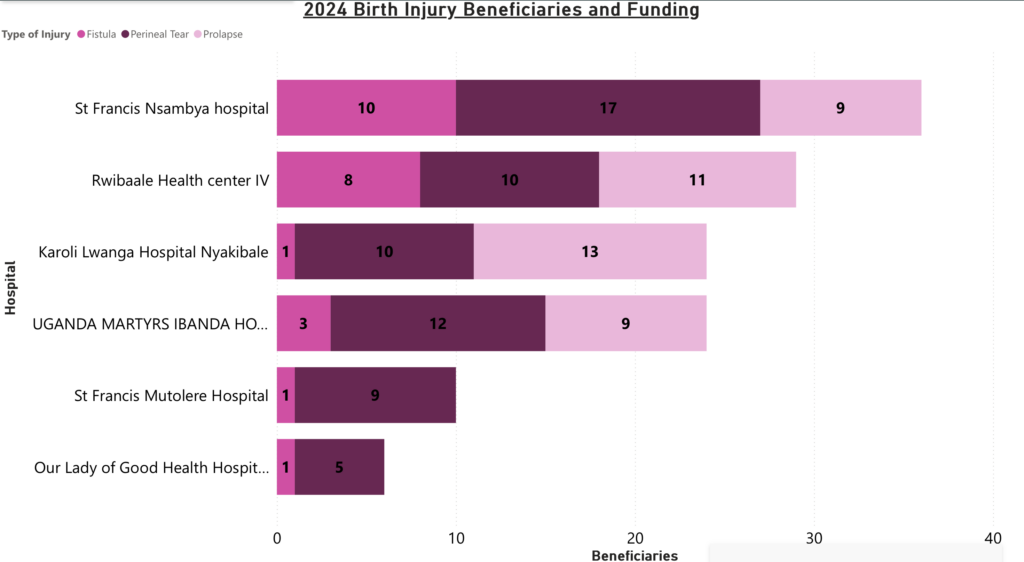
In 2024, African Mission Healthcare, through the SAFE Program, partnered with 6 facilities in Uganda to make corrective birth injury surgeries accessible to women in Uganda. Our goal is to restore dignity, giving women the opportunity to reclaim their lives free from shame and to return to their communities with a renewed sense of purpose and self-worth.
SAFE Program – Improving Access
Financial Access
In areas where AMH works, the per capita income is less than $500 per year. Out-of-pocket health expenditures account for over 40% of the total health expenditure in the country. Many households cannot afford the high upfront costs associated with healthcare, especially for surgical intervention. A single surgical procedure—often costing between $150 and $500, depending on complexity—can represent several months or even a year’s income for a family. This cost is often unaffordable, particularly for subsistence farmers and low-income households, leading to a delay or complete avoidance of treatment.
Human Resource Access
Uganda has fewer than 1.5 healthcare workers per 1,000 people, well below the WHO’s recommendation of 4.45 per 1,000 to ensure effective coverage of essential health services. There are only a handful of surgeons trained to repair birth injuries in the country. Through the birth injury camps, many residents have been trained, who, in due time, will increase coverage.
Geographical Access
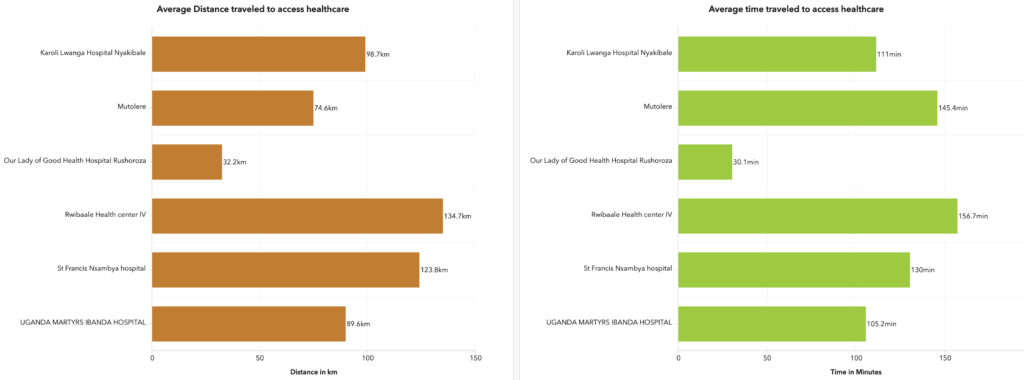
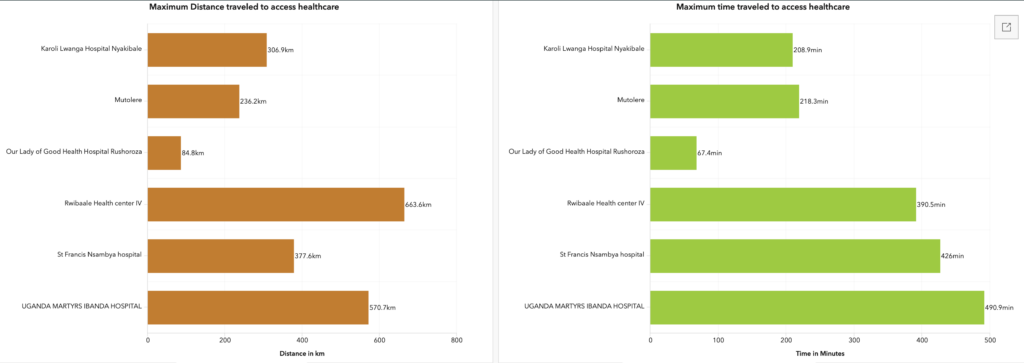
Over 75% of Ugandans live in rural areas, where health facilities are sparsely distributed. This rural population frequently resides more than 5 kilometers from the nearest healthcare center, often only equipped for primary care. The long distances to reach higher-level hospitals, where specialized services such as surgical or emergency obstetric care are available, discourage timely health-seeking behavior, especially for women facing pregnancy-related complications.
2024 Beneficiaries Origin Heatmap
This heatmap illustrates the origins of patients who have traveled, often from considerable distances, to access care at various birth injury camp locations. The bright yellow areas indicate regions with a higher concentration of patients, while the sparser blue areas represent lower patient origin densities.
There is intense clustering of bright yellow near hospitals, suggesting that while these facilities are geographically accessible, many individuals still face insurmountable barriers to care. This pattern highlights a crucial reality: proximity alone does not guarantee access. For many patients, poverty remains a substantial obstacle, limiting their ability to afford transportation, basic medical fees, and essential treatments. This financial barrier leaves patients effectively cut off from services that are nearby but, in practice, out of reach.
Despite African Mission Healthcare’s (AMH) primary focus on western Uganda, this map demonstrates that our efforts are reaching patients from across the country, including central and northern Uganda. Our recent camp at St. Francis Nsambya Hospital in the capital, Kampala, has further extended our reach, allowing us to serve patients from a wider radius. Additionally, our partnerships with facilities in southwestern Uganda attract patients from neighboring countries like Rwanda, underscoring the cross-border impact of our work.


Thanks to the generous support of donors through African Mission Healthcare (AMH), a pathway to healing and dignity has been created. By providing specialized care, we are not just restoring physical health but also rebuilding self-worth and reconnecting women to their communities. Women are reclaiming their roles as mothers, daughters, and leaders within their communities. The impact is profound, breaking the cycle of isolation and stigma and transforming lives for the better.